

Tunneled IPCs were placed in ambulatory setting and patients were discharged on the same day of the procedure. All catheters (PleurX, CareFusion, San Diego, California, USA) were placed in the bronchoscopy unit under moderate sedation by an interventional pulmonologist using ultrasound guidance. Data on patient’s baseline demographics, underlying cancer and stage, type of surgery, catheter side, complications, time of catheter removal, need of subsequent procedures and day of last follow-up were collected. All subjects were required to have undergone at least two therapeutic thoracentesis and have evidence of recurrent pleural effusion prior to consideration for IPC placement. Figure 1 shows schematic representation of patient screening. Eighteen patients had the effusion drained at least twice and 12 had recurrent effusion after second thoracentesis and underwent IPC placement.

All the effusions were exudative in nature and assumed nonmalignant given negative pleural cytology (PET scan was not used as part of the protocol). Thirty-eight of those patients had postoperative symptomatic pleural effusion requiring drainage within the first 90 days post-surgery. A total of 422 patients had lung resection during this time. Treatment plans were decided by a multidisciplinary tumor board and patients received appropriate adjuvant therapy when indicated, electronic medical records for these patients were screened for post-surgical pleural effusion. Patients who underwent lobectomy or segmentectomy as part of the treatment plan for lung cancer between January 2019 and June 2022 were identified. All patients were treated at the University of Florida, a large tertiary academic center in Gainesville, Florida. The study was approved by the institutional ethics review board of the University of Florida (IRB202200492) and individual consent for this retrospective analysis was waived. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
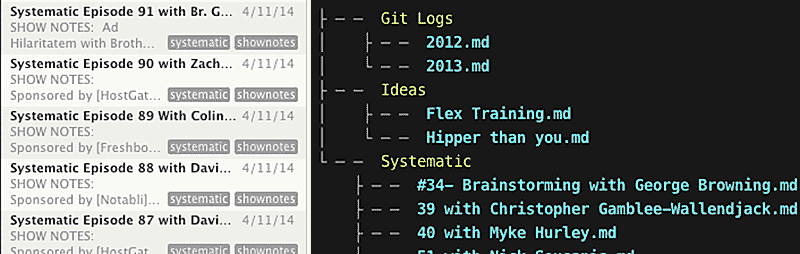
Nvalt persistent note id series#
We present this article in accordance with the AME Case Series reporting checklist (available at ). Secondary outcomes were complications after indwelling catheter placement including infection, dislodgement, pain and bleeding. The primary end points were improved symptomatology and successful pleurodesis leading to removal of catheter. We report our experience of 12 patients with refractory recurrent pleural effusions post lobectomy managed with tunneled IPC. We therefore aimed to present our own experience with this management option and determine whether IPC insertion for recurrent NMPE post lung resection is a feasible and safe alternative.

However, to the best of our knowledge, there is no data regarding the use of IPCs for exudative NMPEs post lung resection.
Other etiologies of NMPE have been successfully treated with an IPC with a low complication rate and high patient satisfaction ( 7, 8). It provides the advantage of shortening length of stay as the procedure can be done in the outpatient setting and can also be used in cases where there is irremediable lung entrapment ( 6). Placement of an IPC with intermittent outpatient drainage by the patient or a patient attendant is an accepted treatment for patients with recurrent malignant effusions ( 4, 5). Consequently, the threshold of intervention such as indwelling pleural catheter (IPC) or pleurodesis is inconsistent and largely at the discretion of the physician and patients’ symptoms. Additionally, effusion size is poorly correlated to symptoms such as dyspnea, vertigo and oxygen demand, as well as to symptom relief after drainage ( 3). The clinical impact of an effusion is not merely dependent on volume, but also on fluid localization, rate of development, concomitant effusions and the patient’s general cardiopulmonary condition. Since the majority of patients with NMPE have significant comorbidities, a multidisciplinary approach is often necessary for management. There are no established guidelines to facilitate management of recurrent NMPE and most management strategies rely on expert experience and data derived from patients with malignancy. Nonmalignant pleural effusions (NMPEs) have a wide variety of etiologies and cause significant morbidity and mortality ( 2). Among the causes, pleural infection, heart failure, and malignancy are the most common. Pleural effusions are diagnosed in about 1.5 million individuals in the United States annually ( 1).


 0 kommentar(er)
0 kommentar(er)
